9 The Price of Patience: Examining Healthcare Waiting Times in Kamloops
The Economic and Social Cost of Wait times for Healthcare in Kamloops
Ashley Thomson
Introduction
Access to timely and efficient healthcare services is a cornerstone of a well-functioning society. However, the city of Kamloops in British Columbia faces a critical healthcare challenge. As of December 12, 2023, a staggering 22,376 Kamloops residents, representing nearly 20% of Kamloops’ population, find themselves on wait lists for family doctors (Munro, 2023). Notably, this does not include people who are not on a waiting list and do not have a family doctor.
When people do not have a family doctor or primary care provider, they often rely on urgent and primary care clinics and hospital emergency rooms to receive the care that would otherwise be provided (Our Care, 2024). These types of spaces are generally designed for emergencies and one-time, quick care. However, many people require ongoing care for a variety of different medical needs, such as diabetes or chronic illnesses. This type of care generally cannot be provided as effectively in these spaces.
Additionally, when these spaces are full of people who require ongoing care, this creates barriers to treating those requiring emergency care (Our Care, 2024). Kamloops currently only has one urgent and primary care clinic and one hospital, making the strain on the local healthcare system substantial. Without access to primary care, Kamloops patients are experiencing significant barriers to treatment. The lack of access to primary care also exacerbates inequalities, as some may be able to afford to pay to travel for care to a place where wait times are shorter. However, this is not an option for many people who require local care. Evidently, the costs of healthcare in Kamloops would be lower if everyone had access to primary care providers and these inefficiencies were avoided.
Past Plan to Address Doctor Shortage
Kamloops residents have long been demanding action be taken to bring more doctors to the city. In the fall of 2022, a group called the Thompson Region Division of Family Practice created a campaign to attract more family doctors to Kamloops. They launched “Champions for Family Medicine,” using financial support from local businesses. The program was forced to end earlier than planned due to a lack of support (Reeve, 2023). The executive director, Tim Shoults, said the group “fell short [in] engaging the business community and getting those cash sponsorships.” Kamloops MLA Peter Milobar emphasized that the government and health authorities should provide proper resources for recruiting and keeping doctors in Kamloops and nearby areas. The failure of this project highlights the need for funding in the process of attracting doctors to Kamloops.
Canada-Wide Healthcare Challenge
Unfortunately, this problem is not unique to Kamloops. All of Canada is facing healthcare challenges. Our Care (2024) reports that about 6.5 million, or 22% of Canadian adults, were without a family doctor as of 2022. They also note an estimated 27% of B.C. adults were without a family doctor (Our Care, 2024). Furthermore, Dandurand et al. (2023) report that “43% of Canadian spine surgeons have noted a wait of over six months for surgery”. With nationwide doctor shortages, national as well as local action must be taken to solve these problems. This commentary will focus on an analysis of Kamloops-specific healthcare wait times and provide suggestions for local action.
Surgery Wait Times
One significant form of treatment Kamloops residents need to access is surgery. Surgery often provides life-altering intervention, improving the quality of life of recipients. A certain amount of waiting time for surgery is necessary, but this waiting time does not come without costs. Furthermore, if wait times become excessive, there are significant negative implications (Landi et al., 2019). Discomfort due to waiting for treatment for a painful condition is just one effect. When wait times are long, outcomes of treatment can be less effective (Ribera et al., 2017). There is a possibility of not qualifying for treatment anymore because of the deterioration of the condition due to the excessive wait time. Most detrimentally, there are links between mortality rates and long waiting times for surgery (Barua et al., 2014; Shojaei et al., 2023). Excessive wait times for surgery may also contribute to negative mental health effects and worse perceptions of health. Mental health effects may include anxiety, depression, and mental isolation. (Barua et al., 2014; Oudhoff et al., 2007; Gagliardi et al., 2021). Additionally, Gagliardi et al. (2021) highlight that excessive waiting may cause distrust in the healthcare system.
Economic Cost
Another significant impact of waiting for surgery is the economic cost. Excessive wait times impose costs on the individual who is waiting as well as on society (Dandurand et al., 2023). One of these costs is the productivity lost when individuals are unable to work while waiting for surgery. Studies, such as Barua and Moir (2023) and Dandurand et al. (2023), have estimated a numerical value for the cost of waiting times for surgery. Barua and Moir (2023) found that waiting for treatment in 2022 costs Canadians an estimated total of $3.6 billion, with an estimated $2,925 per person waiting. This commentary will focus on estimating the cost of the lost productivity of individuals waiting for surgery in Kamloops.
There is a cost associated with any surgery. Some productivity loss, along with other losses, is inevitable. However, excess waiting creates additional costs on top of the costs with a reasonable wait time. Further productivity is lost with a longer wait time, and other additional costs may include increased direct healthcare costs, such as the costs of caring for the waiting person (Fielden et al., 2003). Increased indirect costs, such as the likelihood of more temporary disability benefits needed for the waiting individual, also impose a societal economic cost. The risk of surgery complications becomes higher with a longer wait time, as surgery may be less effective (Ribera et al., 2017). Surgery complications, such as the cost of an additional procedure, would lead to much higher costs. A summary of the economic costs and risks of waiting times, compared to costs and risks without wait times, is presented in Table 1.
Table 1: Other Economic Costs of Surgery With Waiting and No Waiting Time
| Skip Table 1 | ||
| Cost Type | No Waiting Time | With Waiting Time |
|---|---|---|
| Direct Medical Costs |
|
|
| Indirect Costs |
|
|
| Other Costs |
|
|
Note. Summary of data from Barua and Moir (2023), Dandurand et al. (2023), Fielden et al. (2003), and Ribera, et al. (2017).
COVID-19 Impact
The COVID-19 pandemic placed immense strain on healthcare systems worldwide. In Canada, hospitals had to adapt to the changing conditions. Between March 2020 and June 2021, 11% fewer patients were admitted compared to pre-pandemic levels (Gagliardi et al., 2021). Many non-emergency surgical procedures were put on hold due to the influx of COVID-19 patients. This created huge waiting lists for these procedures. A 2020 study by COVIDSurg Collaborative (2020) estimated that over the most disruptive 12 weeks of the COVID-19 pandemic, approximately 28 million surgeries were delayed worldwide. The Canadian Institute for Health Information (2021) estimates that from March 2020 to June 2021, 560,000 fewer surgeries were performed in Canada compared to pre-pandemic levels.
According to the president of the British Columbia Orthopaedic Association, Dr. Lane Dielwart (2022), 1,803 hours, or approximately 900 orthopaedic surgeries, have been lost in Kamloops since the start of the pandemic. Additionally, Kamloops Orthopaedic Surgeon Dr. Scott Hughes stated that 200 surgeries at RIH were cancelled in the two weeks leading up to August 21, 2021 (Mineer, 2021). As we examine the surgery wait times in Kamloops, it is imperative to consider that COVID-19 may still have an impact on the waiting times seen for surgeries today.
Methodology
Surgery Wait Time Data
Surgery wait time data was collected using the British Columbia Ministry of Health’s Surgery Wait Times: Procedures A-Z database (2023). The database lists estimated wait times for each procedure as well as number of people waiting. The data is broken down by health authority and hospital. For this study, data was collected for the Royal Inland Hospital (RIH), which is the only hospital in Kamloops. Data was also collected for wait times across British Columbia. All available procedures for the RIH were included in the analysis. Procedures that listed “N/A” for the wait time at the RIH were excluded from the analysis of B.C. and RIH wait times to allow for direct comparison of procedure wait times. Data that listed “less than 5” people waiting was approximated at two people waiting. Wait times are listed in number of weeks and broken into two categories: “50% of cases completed within,” representing the median wait time for procedures, and “90% of cases completed within,” representing the wait time for 90% of procedures to be completed. The wait times were collected over a three-month period, from August 1, 2023, to October 31, 2023. This date range was used because it was the most recent available data at the time of collection. The number of people waiting for each procedure was reported on October 31, 2023.
Procedure Categories
Wait times were calculated for 23 categories of procedures as well as for all procedures. A breakdown of the categories is listed in Table A4 in the Appendix. The average wait time for 50% of procedures to be completed at RIH was 8.83 weeks, or approximately two months, using 4.33 weeks per month, with a 95% confidence interval [CI] between 6.95 weeks (1.6 months) and 10.72 weeks (2.5 months). This means that half of the surgical procedures took less than two months, and the other half more than two months. B.C.-wide, the average wait time for 50% of procedures to be completed was 7.73 weeks. (1.79 months). The average wait time for 90% of procedures to be completed was 24.95 weeks (5.76 months) at RIH, with a 95% CI between 19.73 weeks (4.56 months) and 30.17 weeks (seven months). This means that 90% of the procedures took less than half a year approximately, but 10% of the procedures took more than half a year of waiting time. B.C.-wide, the average wait time for 90% of procedures to be completed was 29.39 weeks (6.79 months).
Income Data
Income data was collected from Statistics Canada’s 2021 Census Profile (Statistics Canada, 2023). The average gross income in Kamloops in 2020 among recipients was $53,700. The average gross income in B.C. in 2020 among recipients was $54,450 (Statistics Canada, 2023). To calculate average weekly income, 50 weeks per year was estimated to account for two weeks’ vacation. Average weekly income was estimated to be $1,074 in Kamloops and $1,089 in B.C. The time unproductive while waiting for surgery was calculated by multiplying wait times by 13.2%. This is the percentage of time rendered unproductive when waiting for treatment, which was estimated by Barua & Ren (2017). The average unproductive time while waiting for 50% of cases to be completed at RIH was 1.17 weeks. The average unproductive time while waiting for 50% of cases to be completed in B.C. was 1.03 weeks. The average unproductive time while waiting for 90% of cases to be completed at RIH was 3.29 weeks. The average unproductive time while waiting for 90% of cases to be completed in BC was 3.88 weeks. The average wait time was selected to analyze this data, but notably, the median produced very similar results.
Results
Multiplying the estimated unproductive time for all procedures with the average weekly salary gives the estimated cost of waiting for a procedure. For 50% of cases to be completed at RIH, the estimated cost of waiting per procedure was $1,252. In B.C., the estimated cost of waiting per procedure was $1,120. These costs were multiplied by the number of procedures waiting to find the approximate total cost of waiting for procedures. At RIH, 3,086 cases were waiting, and B.C.-wide, 79,635 cases were waiting on October 31, 2023. The estimated total cost of waiting at RIH on October 31, 2023, was $3.9 million. The estimated total cost of waiting in B.C. on October 31, 2023, was $89.2 million. When analyzing the wait times for 90% of procedures to be completed, the estimated cost of waiting per procedure at RIH was $3,537. In B.C., the estimated cost of waiting per procedure was $4,224. The estimated total cost of waiting for 90% of cases to be completed on October 31, 2023, was $10.9 million at RIH and $336.4 million in B.C. Table 2 indicates results broken down by category of surgical procedure for 50% of cases to be completed.
Table 2: Cost of Waiting at RIH vs. BC for 50% of Cases to be Completed
| Skip Table 2 | ||||||
| Procedure Category | RIH Cases Waiting on Oct. 31, 2023 | Average Weeks for 50% of Cases to Be Completed | Weeks Impacted | Cost of Waiting per Case RIH | Cost of Waiting per Case BC | RIH Cost of Waiting All Cases |
|---|---|---|---|---|---|---|
| Biopsy in OR | 5 | 1.40 | 0.18 | $198 | $474 | $992 |
| Breast | 121 | 12.93 | 1.71 | $1,832 | $909 | $221,715 |
| Cyst/Ganglion Removal | 10 | 7.60 | 1.00 | $1,077 | $920 | $10,774 |
| Dental Surgery | 51 | 12.30 | 1.62 | $1,744 | $1,653 | $88,931 |
| Ears | 18 | 13.60 | 1.80 | $1,928 | $3,464 | $34,705 |
| Excision Lesion/Tumour | 26 | 2.90 | 0.38 | $411 | $647 | $10,689 |
| Eyes | 590 | 3.70 | 0.49 | $525 | $862 | $309,480 |
| Gastrointestinal/Digestive System | 79 | 10.93 | 1.44 | $1,550 | $839 | $122,450 |
| Gynaecology | 156 | 6.68 | 0.88 | $946 | $1,143 | $147,623 |
| Head | 69 | 10.63 | 1.40 | $1,507 | $1,461 | $104,015 |
| Hernia | 201 | 14.20 | 1.87 | $2,013 | $1,358 | $404,634 |
| Joint/Muscle/Bone | 1074 | 8.63 | 1.14 | $1,223 | $1,418 | $1,313,232 |
| Liver/Pancreas | 55 | 5.40 | 0.71 | $766 | $805 | $42,105 |
| Nasal Surgery | 40 | 23.30 | 3.08 | $3,303 | $3,177 | $132,128 |
| Neck/Throat | 46 | 14.95 | 1.97 | $2,119 | $1,747 | $97,494 |
| Nerve Surgery | 122 | 29.40 | 3.88 | $4,168 | $733 | $508,493 |
| Prostate Surgery | 129 | 9.90 | 1.31 | $1,404 | $862 | $181,052 |
| Skin | 18 | 4.10 | 0.54 | $581 | $589 | $10,462 |
| Spinal/Back Surgery | 124 | 7.40 | 0.98 | $1,049 | $862 | $130,086 |
| Urinary Tract | 97 | 8.40 | 1.11 | $1,191 | $594 | $115,513 |
| Vascular System | 8 | 1.18 | 0.16 | $167 | $474 | $1,333 |
| Wound/Laceration Care | 7 | 1.00 | 0.13 | $142 | $374 | $992 |
| Other Procedures | 40 | 3.65 | 0.48 | $517 | $668 | $20,698 |
Note. Calculations done using data from British Columbia Ministry of Health (2023) and Statistics Canada (2023).
Discussion & Comparison
On average, surgery wait time in Kamloops is about one week longer than the average BC wait time. Furthermore, the average cost of waiting per case in Kamloops is about $132 higher than the B.C.-wide average cost of waiting per case. This may be attributed to the larger concentration of doctors and surgeons in the Vancouver Metropolitan area, where much of the population of BC is concentrated. Comparing the analysis in this study to a similar study conducted by Barua & Moir (2023) with the Fraser Institute, the latter produces a much higher cost of waiting. The estimated cost per procedure in BC in 2022 was $2,363, according to Barua & Moir (2023). However, their result is based on the wait time from consultation with a specialist until the treatment is complete, while this study estimates wait time from when the surgery is booked until when it is complete.
Comparing this study to Dandurand et al. (2023), the latter included direct healthcare utilization costs and the indirect cost of lost work. The indirect cost of lost work was calculated using average income and the amount of work missed by each subject. Dandurand et al. (2023) used data on the actual missed work time for each subject, whereas this study used an average estimate of unproductive time.
To reduce the cost of waiting for surgery in Kamloops, the health authority may consider prioritizing reducing the wait lists for those procedures which have the most people waiting (cataract surgery, knee replacement, hernia repair) and those which have the longest wait times (nerve surgery, breast reduction, tonsillectomy/adenoidectomy). However, to effectively prioritize, the severity of each condition being treated should also be considered (Oudhoff et al., 2007). Attracting doctors to Kamloops, especially family doctors and surgeons, will also help alleviate the costs of long wait times. Prioritizing attracting surgeons who specialize in the procedures with the longest wait times may be an effective method of targeting those wait lists. Reducing the wait lists for family doctors will help reduce overall healthcare wait times in Kamloops and reduce the cost of waiting that takes place before a surgery is booked, which was not measured in this study but also poses an individual cost (Barua & Moir, 2023).
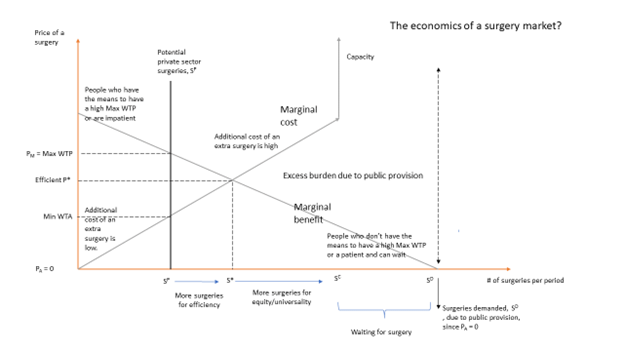
A Simple Model of Surgery Wait Times
This section illustrates how waiting times evolve in a public-provided healthcare system. For every surgery, there is a marginal benefit associated with or a maximum amount someone is willing to pay for surgery. It is assumed that the marginal benefit of an extra surgery to an extra person in each period decreases as the number of surgeries to people increases. The reduction in the maximum amount someone is willing to pay is driven by income, amongst other factors such as the type of surgery (e.g. knee or hip replacement surgery, cosmetic). The marginal cost is upward-sloping. As the number of surgeries increases, it becomes more expensive to add an additional surgery.
In a perfectly competitive market, the outcome of providing surgeries is at level S*, where the marginal cost is equal to the marginal benefit for the extra surgery. The market would find an equilibrium price of the surgery at P*. At this level, many people want surgeries, but these surgeries will not be provided to them, nor will they be on a waiting list. Only those who value the surgeries more and are “willing to pay” more to have a surgery than the marginal cost of provision will be exchanged. However, if the market is not competitive, then the price will be even higher than P* at PM, reducing the number of surgeries even further to SP and creating an inefficient healthcare system since mutually beneficial exchanges between patients and private health facilities are disallowed. Some patients who have income and cannot wait will pay PM to have the surgery, either in a private clinic in Canada or another country like the United States.
Canada has a public healthcare system that provides surgery to almost everyone who needs one within capacity constraints. In Figure 1, capacity constrain is reached at SC. However, the number of surgeries demanded is at SD in each period since the price per surgery is zero. Everyone who needs surgery will want one because the marginal benefit of surgery is positive, no matter how low it is. At this point, the quantity demanded for surgeries exceeds the capacity of the public health care system to provide surgeries, and an excess burden evolves due to the public provision with people waiting to have surgery. Thus, the public healthcare system ends up with a high waiting list because of limited resources, resulting in capacity constraints, and the number of surgeries is less than SD in each period.
The difference between SD and SC is the amount of people on the waiting list. A private market would never operate in a region of more than S* surgeries and more likely to operate in a region of less than S* if firms had some monopoly power. The public healthcare sector should strive to increase surgeries by more than S* in each period and attempt to reach capacity between SD and S*. One serious problem with a market system allocation is that it depends on those who have the income to pay for the surgery and does not account for the severity of the situation, which is discussed in the next section. The public healthcare system can allocate surgeries to those who have a severe situation but cannot afford to pay a lot due to income constraints.
Alternative Strategies for Surgeries & Wait Times
Allocating Surgeries
An appropriate way to allocate surgeries is a system of prioritization. Prioritization based on the severity of the condition would allow for treatment of severe conditions first and would potentially leave patients with less negative effects of waiting for surgery. Another prioritization method could be using a scoring system, such as the Medically Necessary, Time-Sensitive (MeNTS) system (Prachand et al., 2020), or a modified version that is weighted, which was developed by Rana et al. (2022). This prioritization system scores based on factors related to the procedure, disease, and patient (Rana et al., 2022). However, these methods may not reduce the waiting times.
Reducing Waiting Times
Public concern about wait times can prompt actions to improve timely access to healthcare services (Gregory et al., 2013; Segall et al., 2020). Studies like Saunders & Carter (2017) examine a public-private hospital partnership in New South Wales, finding that transferring 15% of public rehab bed days to private hospitals ensured timely elective surgeries for public patients. They advocate for a strategic, research-supported approach to manage hospital capacities and reduce wait times. Public waiting times can be reduced by effective demand-side policies that incentivize patients (e.g., providing subsidies) to opt out of the public system, shifting demand to the private market (Chen et al., 2015). This would allow for less strain on the public healthcare system and allow people who have the means to access the private system to do so.
Additionally, socioeconomic factors do not seem to influence surgical wait times in public systems significantly, indicating equitable access to surgical care across socioeconomic status (Law et al., 2022). A study advocates for adopting single-entry models and team-based care to manage waiting times, presenting these approaches as efficient, fair, and ethical solutions that improve care standardization and surgeons’ work environments. Despite some resistance from surgeons due to concerns about autonomy and financial security, the widespread adoption of these models for a broader transformation of the healthcare system is encouraged (Urbach, 2018; Urbach and Martin, 2020).
Limitations & Conclusion
This research determines the cost of waiting for surgery based on an approach that places a value on the lost productivity of individuals unable to work. An estimate of an average work week was used, and income data is from 2020. Data for the study was collected for the Royal Inland Hospital and may include patients who do not reside in Kamloops but who travelled to receive their care. Because estimates were used in calculating the lost productivity, these results should be interpreted with caution. The economic cost of surgery wait time in this study is based on the wait time from when a surgery is scheduled until the procedure is complete. Dr. Jill Calder, former Director of Rehabilitation Services at the Royal Inland Hospital, states that “the real wait times are from the moment the patient is recognized to need surgery, which is way before the “waitlist” from the hospital perspective” (J. Calder, personal communication, April 20, 2024). When including the wait from when a patient is recognized to need surgery, costs would likely be much higher. Time for scheduling doctor’s appointments and any other appointments needed before surgery would add significant waiting time and would increase costs.
In addition to not capturing the entire length of waiting time, this valuation cannot account for the cost of lost homemaking work, lost productivity due to family care, or the lost leisure and social time due to waiting for surgery. Additionally, this study does not include the direct costs of healthcare, such as treatment and surgery costs. Therefore, the true cost of waiting for surgery in Kamloops is likely much higher than the estimated value in this chapter. With such a high estimated economic cost of waiting for surgery in Kamloops, it would be very beneficial for the community to have better access to family doctors, more surgeons, and shorter wait lists.
Media Attributions
Figure 1: “A market model illustrating issues of efficiency versus equity” by the author is under a CC BY-NC-SA 4.0 license.
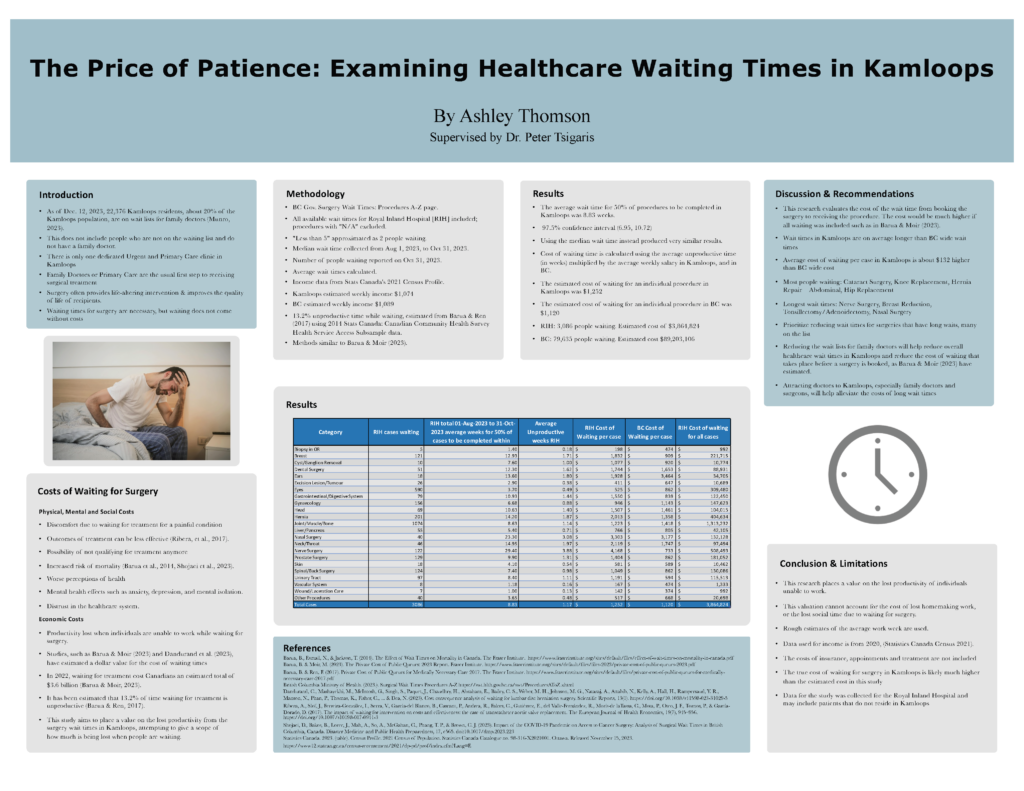
Figure 2: “Ashley Thomson’s poster presentation at the 19th Undergraduate Research Conference during March 2024” by the author is under a CC BY-NC-SA 4.0 license.
References
Barua, B., Esmail, N., & Jackson, T. (2014). The effect of wait times on mortality in Canada. Fraser Institute. https://www.fraserinstitute.org/sites/default/files/effect-of-wait-times-on-mortality-in-canada.pdf
Barua, B. & Ren, F. (2017). The private cost of public queues for medically necessary care 2017. Fraser Institute. https://www.fraserinstitute.org/sites/default/files/private-cost-of-public-queues-for-medically-necessary-care-2017.pdf
British Columbia Ministry of Health. (n.d.). Surgical wait times: Procedures a-z. Government of British Columbia. https://swt.hlth.gov.bc.ca/swt/ProceduresAToZ.xhtml
Canadian Institute for Health Information. (2021). COVID-19’s impact on hospital services. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/hospital-services
Chen, H., Qian, Q., & Zhang, A. (2015). Would allowing privately funded health care reduce public waiting time? Theory and empirical evidence from Canadian joint replacement surgery data. Production and Operations Management, 24(4), 605–618. https://doi.org/10.1111/poms.12260
COVIDSurg Collaborative. (2020). Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. British Journal of Surgery, 107(11), 1440–1449. https://doi.org/10.1002/bjs.11746
Dandurand, C., Mashayekhi, M. S., McIntosh, G., Singh, S., Paquet, J., Chaudhry, H., Abraham, E., Bailey, C. S., Weber, M. H., Johnson, M. G., Nataraj, A., Attabib, N., Kelly, A., Hall, H., Rampersaud, Y. R., Manson, N., Phan, P., Thomas, K., Fisher, C., … & Dea, N. (2023). Cost consequence analysis of waiting for lumbar disc herniation surgery. Scientific Reports, 13, Article No. 4519. https://doi.org/10.1038/s41598-023-31029-5
Dielwart, C. L. (2022, March 16). Letter from BCOA to the BC Health Minister – March 16, 2022. In Information for patients: Wait times for surgery. British Columbia Orthopaedic Association. https://bcoa.ca/information-for-patients/wait-times-for-surgery/
Fielden, J., Cumming, J. M., Horne, J. G., Devane, P. A., Slack, A., & Gallagher, L. M. (2005). Waiting for hip arthroplasty: Economic costs and health outcomes. The Journal of Arthroplasty, 20(8), 990–997. http://doi.org/10.1016/J.ARTH.2004.12.060
Gagliardi, A. R., Yip, C. Y. Y., Irish, J., Wright, F. C., Rubin, B., Ross, H., Green, R., Abbey, S., McAndrews, M. P., & Steward, D. E. (2021). The psychological burden of waiting for procedures and patient‐centred strategies that could support the mental health of wait‐listed patients and caregivers during the COVID‐19 pandemic: A scoping review. Health Expectations, 24(3), 978–990. https://doi.org/10.1111/hex.13241
Gregory, D. M., Newhook, J. T., & Twells, L. K. (2013). Patients’ perceptions of waiting for bariatric surgery: A qualitative study. International Journal for Equity in Health, 12, Article No. 86. https://doi.org/10.1186/1475-9276-12-86
Landi, S., Ivaldi, E., & Testi, A. (2019). Socioeconomic status and waiting times for health services: Current evidences and next area of research. Health Services Insights, 12. https://doi.org/10.1177/1178632919871295
Law, T. J., Stephens, D., & Wright, J. G. (2022). Surgical wait times and socioeconomic status in a public healthcare system: a retrospective analysis. BMC Health Services Research, 22, Article No. 579. https://doi.org/10.1186/s12913-022-07976-6
Mineer, B. (2021, August 23). More than 200 elective surgeries reportedly cancelled at Royal Inland Hospital due staff shortages. Radio NL. https://www.radionl.com/2021/08/23/more-than-200-elective-surgeries-reportedly-cancelled-at-royal-inland-hospital-due-staff-shortages/
Moir, M., & Barua, B. (2023). The private cost of public queues for medically necessary care, 2023. Fraser Institute. https://www.fraserinstitute.org/sites/default/files/2023-private-cost-of-public-queues.pdf
Munro, R. (2023, December 19). Almost half of those in Interior Health waiting for a family doctor are in Kamloops. INFOnews. https://infotel.ca/newsitem/almost-half-of-those-in-interior-health-waiting-for-a-family-doctor-are-in-kamloops/it102198
Oudhoff, J. P., Timmermans, D. R. M., Knol, D. L., Bijnen, A. B., & van der Wal, G. (2007). Waiting for elective general surgery: Impact on health related quality of life and psychosocial consequences. BMC Public Health, 7, Article No. 164. https://doi.org/10.1186/1471-2458-7-164
OurCare. (2024). Primary care needs OurCare: The final report of the largest pan-Canadian conversation about primary care. MAP Centre for Urban Health Solutions. https://issuu.com/dfcm/docs/primary_care_needs_ourcare_the_final_report_of_the?fr=xKAE9_zU1NQ
Prachand, V. N., Milner, R., Angelos, P., Posner, M. C., Fung, J. J., Agrawal, N., Jeevanandam, V., & Matthews, J. B. (2020). Medically necessary, time-sensitive procedures: Scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. Journal of the American College of Surgeons, 231(2), 281–288. https://doi.org/10.1016/j.jamcollsurg.2020.04.011
Rana, H. S., Umer, M., Hassan, U., & Asgher, U. (2022). A novel multi-criteria decision-making approach for prioritization of elective surgeries through formulation of “weighted MeNTS scoring system”. Heliyon, 8(8). Article No. e10339. https://doi.org/10.1016/j.heliyon.2022.e10339
Reeve, M. (2023, January 25). Kamloops family doctor recruitment campaign comes to an early end. CFJC Today. https://cfjctoday.com/2023/01/25/kamloops-family-doctor-recruitment-campaign-comes-to-an-early-end/
Ribera, A., Slof, J., Ferreira-González, I., Serra, V., García-del Blanco, B., Cascant, P., Andrea, R., Falces, C., Gutiérrez, E., del Valle-Fernández, R., Morís-de laTassa, C., Mota, P., Oteo, J. F., Tornos, P., & García-Dorado, D. (2017). The impact of waiting for intervention on costs and effectiveness: The case of transcatheter aortic valve replacement. The European Journal of Health Economics, 19, 945–956. https://doi.org/10.1007/s10198-017-0941-3
Saunders, C., & Carter, D. (2017). Right care, right place, right time: Improving the timeliness of health care in New South Wales through a public–private hospital partnership. Australian Health Review, 41(5), 511–518. https://doi.org/10.1071/ah16075
Segall, R. E., Takata, J. L., & Urbach, D. R. (2020). Wait-time reporting systems for elective surgery in Canada: A content analysis of provincial and territorial initiatives. CMAJ Open, 8(4), E844–E851. https://doi.org/10.9778/cmajo.20200033
Shojaei, D., Bakos, B., Loree, J., Mah, A., So, A., McGahan, C., Phang, T. P., & Brown, C. J. (2023). Impact of the COVID-19 pandemic on access to cancer surgery: Analysis of surgical wait times in British Columbia, Canada. Disaster Medicine and Public Health Preparedness, 17, Article No. e565. https://doi.org/10.1017/dmp.2023.223
Statistics Canada. (2023). Census profile, 2021 census of population (No. 98-316-X2021001) [Table]. https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/index.cfm?Lang=E
Urbach, D. R. (2018). Improving access to health services in Canada. Healthcare Management Forum, 31(6), 256–260. https://doi.org/10.1177/0840470418776995
Urbach, D. R., & Martin, D. (2020). Confronting the COVID-19 surgery crisis: time for transformational change. Canadian Medical Association Journal, 192(21), E585–E586. https://doi.org/10.1503/cmaj.200791
Appendix
| Skip Table A1 | ||||
| Category | BC Cases Waiting on Oct. 31, 2023 |
Average Weeks for 50% of Cases to Be Completed | Unproductive Weeks | Cost of Waiting per Case |
|---|---|---|---|---|
| Biopsy in OR | 390 | 3.30 | 0.44 | $474 |
| Breast | 2921 | 6.33 | 0.83 | $909 |
| Cyst/Ganglion Removal | 381 | 6.40 | 0.84 | $920 |
| Dental Surgery | 1252 | 11.50 | 1.52 | $1,653 |
| Ears | 622 | 24.10 | 3.18 | $3,464 |
| Excision Lesion/Tumour | 768 | 4.50 | 0.59 | $647 |
| Eyes | 17776 | 6.00 | 0.79 | $862 |
| Gastrointestinal/Digestive System | 1536 | 5.83 | 0.77 | $839 |
| Gynaecology | 7546 | 7.95 | 1.05 | $1,143 |
| Head | 1913 | 10.17 | 1.34 | $1,461 |
| Hernia | 5171 | 9.45 | 1.25 | $1,358 |
| Joint/Muscle/Bone | 22976 | 9.87 | 1.30 | $1,418 |
| Liver/Pancreas | 1519 | 5.60 | 0.74 | $805 |
| Nasal Surgery | 3044 | 22.10 | 2.92 | $3,177 |
| Neck/Throat | 1333 | 12.15 | 1.60 | $1,747 |
| Nerve Surgery | 340 | 5.10 | 0.67 | $733 |
| Prostate Surgery | 1697 | 6.00 | 0.79 | $862 |
| Skin | 1336 | 4.10 | 0.54 | $589 |
| Spinal/Back Surgery | 1540 | 6.00 | 0.79 | $862 |
| Urinary Tract | 2510 | 4.13 | 0.55 | $594 |
| Vascular System | 539 | 3.30 | 0.44 | $474 |
| Wound/Laceration Care | 262 | 2.60 | 0.34 | $374 |
| Other Procedures | 2263 | 4.65 | 0.61 | $668 |
| Total Cases In B.C. | 79635 | 7.79 | 1.03 | $1,120 |
Note. Calculations done using data from British Columbia Ministry of Health (2023) and Statistics Canada (2023).
| Skip Table A2 | |||||
| Category | RIH Cases Waiting on Oct. 31, 2023 |
Average Weeks for 90% of Cases to Be Completed | Unproductive Weeks | Cost of Waiting per Case | RIH Cost of Waiting for All Cases |
|---|---|---|---|---|---|
| Biopsy in OR | 5 | 17.90 | 2.36 | $2,538 | $12,688 |
| Breast | 121 | 5.10 | 0.67 | $723 | $87,485 |
| Cyst/Ganglion Removal | 10 | 33.15 | 4.38 | $4,700 | $46,996 |
| Dental Surgery | 51 | 11.40 | 1.50 | $1,616 | $82,424 |
| Ears | 18 | 23.70 | 3.13 | $3,360 | $60,478 |
| Excision Lesion/Tumour | 26 | 27.60 | 3.64 | $3,913 | $101,733 |
| Eyes | 590 | 7.90 | 1.04 | $1,120 | $660,781 |
| Gastrointestinal/Digestive System | 79 | 17.90 | 2.36 | $2,538 | $200,474 |
| Gynaecology | 156 | 45.37 | 5.99 | $6,432 | $1,003,320 |
| Head | 69 | 22.43 | 2.96 | $3,179 | $219,361 |
| Hernia | 201 | 20.17 | 2.66 | $2,859 | $574,657 |
| Joint/Muscle/Bone | 1074 | 40.70 | 5.37 | $5,770 | $6,196,934 |
| Liver/Pancreas | 55 | 30.98 | 4.09 | $4,392 | $241,584 |
| Nasal Surgery | 40 | 24.00 | 3.17 | $3,402 | $136,097 |
| Neck/Throat | 46 | 40.10 | 5.29 | $5,685 | $261,505 |
| Nerve Surgery | 122 | 24.45 | 3.23 | $3,466 | $422,880 |
| Prostate Surgery | 129 | 41.80 | 5.52 | $5,926 | $764,441 |
| Skin | 18 | 37.90 | 5.00 | $5,373 | $96,714 |
| Spinal/Back Surgery | 124 | 8.05 | 1.06 | $1,141 | $141,513 |
| Urinary Tract | 97 | 17.80 | 2.35 | $2,523 | $244,777 |
| Vascular System | 8 | 25.20 | 3.33 | $3,573 | $28,580 |
| Wound/Laceration Care | 7 | 3.65 | 0.48 | $517 | $3,622 |
| Other Procedures | 40 | 3.90 | 0.51 | $553 | $22,116 |
| Total Cases | 3086 | 24.95 | 3.29 | $3,537 | $10,914,288 |
Note. Calculations done using data from British Columbia Ministry of Health (2023) and Statistics Canada (2023).
| Skip Table A3 | ||||
| Category | BC Cases Waiting on Oct. 31, 2023 |
Average Weeks for 90% of Cases to Be Completed | Unproductive Weeks | Cost of Waiting per Case |
|---|---|---|---|---|
| Biopsy in OR | 390 | 20.70 | 2.73 | $2,976 |
| Breast | 2921 | 13.50 | 1.78 | $1,941 |
| Cyst/Ganglion Removal | 381 | 28.25 | 3.73 | $4,061 |
| Dental Surgery | 1252 | 26.70 | 3.52 | $3,838 |
| Ears | 622 | 76.50 | 10.10 | $10,997 |
| Excision Lesion/Tumour | 768 | 17.10 | 2.26 | $2,458 |
| Eyes | 17776 | 22.70 | 3.00 | $3,263 |
| Gastrointestinal/Digestive System | 1536 | 22.20 | 2.93 | $3,191 |
| Gynaecology | 7546 | 28.43 | 3.75 | $4,086 |
| Head | 1913 | 34.93 | 4.61 | $5,022 |
| Hernia | 5171 | 42.65 | 5.63 | $6,131 |
| Joint/Muscle/Bone | 22976 | 34.99 | 4.62 | $5,030 |
| Liver/Pancreas | 1519 | 20.10 | 2.65 | $2,889 |
| Nasal Surgery | 3044 | 24.00 | 3.17 | $3,450 |
| Neck/Throat | 1333 | 36.55 | 4.82 | $5,254 |
| Nerve Surgery | 340 | 37.60 | 4.96 | $5,405 |
| Prostate Surgery | 1697 | 38.20 | 5.04 | $5,491 |
| Skin | 1336 | 48.10 | 6.35 | $6,914 |
| Spinal/Back Surgery | 1540 | 28.25 | 3.73 | $4,061 |
| Urinary Tract | 2510 | 34.40 | 4.54 | $4,945 |
| Vascular System | 539 | 15.23 | 2.01 | $2,190 |
| Wound/Laceration Care | 262 | 15.63 | 2.06 | $2,246 |
| Other Procedures | 2263 | 16.10 | 2.13 | $2,314 |
| Total Cases In BC | 79635 | 29.39 | 3.88 | $4,224 |
Note. Calculations done using data from British Columbia Ministry of Health (2023) and Statistics Canada (2023).
| Skip Table A4 | |
| Category | Procedure Types |
|---|---|
| Other Procedures | All other procedures; Laparoscopy |
| Biopsy in OR | Biopsy in OR |
| Breast | Breast biopsy; Breast reconstruction; Breast reduction; Mastectomy |
| Cyst/Ganglion Removal | Cyst/Ganglion removal |
| Dental Surgery | Dental surgery |
| Ears | Tympanoplasty |
| Excision Lesion/Tumour | Excision lesion/Tumour |
| Eyes | Cataract surgery |
| Gastrointestinal/Digestive System | Bowel resection; Colostomy/Ileostomy; Rectal surgery |
| Gynaecology | D&C and related surgery; Fallopian tube/Ovarian surgery; Uterine surgery; Vaginal Repair |
| Head | Cranial surgery; Parotidectomy; Sinus surgery |
| Hernia | Hernia repair — Abdominal; Hernia repair — Hiatal |
| Joint/Muscle/Bone | Foot/Ankle surgery; Fracture repair; Hand/Wrist surgery; Hip replacement; Knee — ACL Repair; Knee — Meniscectomy; Knee arthroscopy; Knee replacement; Other joint reconstruction; Other orthopaedic surgery; Shoulder surgery; Tendon surgery |
| Liver/Pancreas | Cholecystectomy |
| Nasal Surgery | Nasal surgery |
| Neck/Throat | Thyroidectomy; Tonsillectomy/Adenoidectomy |
| Nerve Surgery | Nerve surgery |
| Prostate Surgery | Prostate surgery |
| Skin | Skin surgery; Skin tumour removal |
| Spine/Nerves | Spinal/Back surgery |
| Urinary Tract | Bladder surgery; Kidney/Bladder stone removal; Other urology surgery |
| Vascular System | Aortic aneurysm repair; Endarterectomy; Vascular bypass graft — Non Cardiac; Vascular surgery — Other |
| Wound/Laceration Care | Wound/Laceration care |

